The Surprising Connection between the Gut Microbiome and Infections in other Organs
Part 2 in a 7 part series: For king and country – tend to your immune system
This article was originally published as a guest editor post at foodpharmacy.se
By: Graeme Jones, clinical physiologist and CEO at Nordic Clinic Stockholm.
Published: 15/04/2020
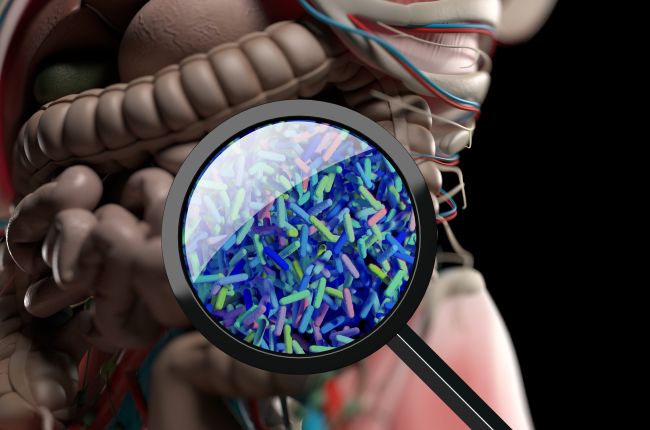
Extensive research is currently underway looking at the role that the gut microbiota – all the microorganisms in the intestinal tract – plays in overall health. As we’ll learn in this article, there is a link between the gut flora and immune health. But let’s start with the connections found between gut microbiota and brain health.
In the early stages of gut microbiome research, scientists linked gut health to brain health through a major communication ‘highway’ called the vagus nerve, which travels from the digestive tract to the brain (think of it like a direct telephone line). This nerve, which influences everything from our mood to our immune response, digestion and heart rate, exerts a relaxation effect – it slows your heart rate, decreases blood pressure, improves your mood and coordinates digestion. “Sign me up for more of that”, I hear you say, “can I install a second telephone line?” Well no, sorry, but we can stimulate it through various techniques – more on that later. That is why it has been the target of treatment for major depression, post traumatic stress disorder and inflammatory bowel disease, amongst others. It has also shown as a conduit through which the gut microbiota mediates effects on the brain. So our digestive bacteria ‘talk’ to our brain through this direct ‘phone line’? Bullseye!
With the continuous and alarming escalation of dementia worldwide and no pharmaceutical cure in the pipeline (many pharmaceutical companies have just completely dropped the development of Alzheimer’s medication), of great interest are further reports that the microbiota play a role in the pathogenic cascade of both Parkinson and Alzheimer diseases (1). With all this research, it has led to a commonly accepted term called the gut-brain axis, but we are now discovering this was barely a scratching of the surface. While scientists were digging into this axis, they discovered many more communication ‘highways’ or ‘axes’, where information travels back and forth to coordinate a whole host of activities in the body. Some of these bi-directional axes include:
- Gut-liver axis
- Gut-bone axis
- Gut-immune axis
- Gut-muscle axis
- Gut-fat axis
- Gut-lung axis
- Gut-heart axis
Could these billions of bacteria living in our gut play a role in how distant organs and tissues function? Yes, it seems! The vagus nerve ‘direct line’ is only one part of this puzzle, so let’s dive into some of the other communication tools these sneaky little bugs use in our intestinal tract.
Our microbes mobile phone equivalent
If we think of the gut bacteria influencing the vagus nerve as a sort of ‘old school direct telephone cable line’ to the brain, then what other methods of communication can they use across the different axes? By-products produced by the microbes in our intestines are called microbial metabolites and they are released from the gut. They include two key metabolites called secondary bile acids and short-chain fatty acids. Think of these like using a mobile phone network instead of a direct line to communicate with different tissues. The first, bile acids, break down and aid absorption of fat from our diet whilst the second, short-chain fatty acids, are produced by beneficial bacteria when we eat fibre and make their way to the brain. This is one of the reasons why a high fibre diet could be very important for brain health.
Gut-Immune Axis
As we are discovering, these gut microbes have different communication channels they can pull on to talk to the different tissues. Since the gut microbiome also has a powerful effect on the immune system via the gut-immune axis, might this whopping 2 kg of microbes living in our intestines help modulate infection risk in some of these other tissues? Let’s look at some of these connections.
The Heart
Myocarditis is inflammation of the heart and typically occurs due to viral infection. Using mouse models of autoimmune myocarditis, researchers have discovered that modulating the gut microbiome may be a novel target for improving outcomes (2).
Another paper found that excessively activating immune cells in the gut exacerbates myocarditis in mice, progressing to mortality (3). Additionally, T cells (an important part of our immune defence system) in humans with myocarditis were more reactive to Bacteroides thetaiotaomicron (a common bacteria found in the gut) than those from healthy controls. This data implies that mortality from myocarditis may be partly regulated by the state of the microbial ecosystem in the gut.
Lung infections
Viral respiratory infection severity often worsens with secondary infections that may arise from the gut. A study in mice found that influenza A infection causes changes in the gut microbiome that, upon transfer to healthy mice, impairs defense to pneumococcal infection (4). Pneumococcal infection is caused by a type of bacteria called streptococcus pneumoniae, which can affect the lungs – now you know why it is called pneumonia. This means that in mouse models, getting the flu can cause changes in the gut bacteria and this subsequently decreases defence to a lung infection.
In older humans it has been shown that antibiotic treatment alters immunity to vaccination by decreasing specific influenza antibodies (5), meaning antibiotics may decrease our ability to fight influenza viruses as we get older. Interestingly, treatment with antibiotics increased the inflammatory response through loss of secondary bile acids (which I talked about earlier in this article) created by members of the gut microbiome.
Bloodstream infections (BSI)
For decades, some brave souls in medicine have been pushing for more research into whether ‘leaky gut’, describing the translocation of bacteria from the intestine into the bloodstream, actually occurs. The standard medical establishment has viewed this as quackery, until research has slowly caught up actually showing this can and does happen under various disease states and circumstances such as type II diabetes, high fat diets and alcohol consumption, to name a few. At Nordic Clinic, where we deal with patients who suffer from chronic health conditions, in subsets of patients we can often test and find they have resident bacteria from the oral and digestive cavity present in the bloodstream!
One of the most severe and worrying conditions I can think of is sepsis, where the body’s response to infection causes injury to its tissues and organs. Several studies have successfully used tests to show bacterial and fungal toxins from the gut present in the bloodstream, mostly in patients with this condition (7). And intestinal barrier dysfunction, where the digestive tract becomes hyperpermeable (a better term for ‘leaky gut’), is thought to contribute to the development of multiple organ dysfunction syndrome in sepsis (8).
Enhanced levels of bacterial toxins are also found in patients with obesity and metabolic syndrome (9,10) which might indicate bacterial translocation from the gut lumen into circulation as a consequence of intestinal barrier function failure causing ‘leaky gut’. As I say time and time again, looking after your metabolic health is so important for gut health and vice versa.
Middle Ear Infections in children
Many parents I am sure can relate to spending hours at the doctor’s surgery for their child’s ear infections. It is caused by bacteria that travel and make their way from the upper part of the throat, through canals (called Eustachian tubes), to the middle ear. Symptoms include fever, earache, and occasionally the eardrum may perforate, discharging pus into the ear canal.
Antibiotics are often prescribed for acute middle ear infection, although they have only a modest effect on reducing symptoms. Moreover, excessive antibiotic use leads to antibiotic resistance (a very worrying side-effect of use), making them less effective for these and other possible future infections. Consequently, preventing acute middle ear infection is highly desirable over treatment. According to Cochrane Reviews website, whose work is internationally recognized as the benchmark for high-quality information about the effectiveness of healthcare, probiotics may prevent ear infections in children not prone to it (11). This suggests there is a possible link between a substance (probiotic bacteria) that modulates the gut microbiome and the prevention of ear infections.
Urinary Tract
UTI (Urinary Tract Infection), is one of the most common types of infection affecting over 150 million people yearly (12). A recent study found that digestive tract abundances of Escherichia and Enterococcus (families of bacteria that live in the gut) are associated with future development of Escherichia and Enterococcus urinary tract infection, respectively, independent of clinical factors like gender (13). These microbes do not seem to discriminate between the sexes, and the gut seems to be the ‘headquarters’ from which infection can possibly arise.
Reduce the risk of infection by cultivating a healthy gut microbiome
By various methods, our gut microbes are able to communicate with a whole variety of tissues, organs and glands. A large body of research evidence is growing demonstrating how important it is to have optimal gut health, function, bacterial balance, and a robust intestinal barrier to ensure a reduced risk of many other types of infection, syndromes and diseases. A viable strategy may be that we all should be monitoring our gut microbial communities on a yearly basis, like we do with our cars as they age – it is always more effective to prevent rather than cure.
Infection has and will continue to happen to all of us, it is an inevitable part of being alive in this biodiverse ecosystem we call Earth. However, we can possibly reduce our risk of infection, or infection being very problematic, by cultivating our own healthy gut microbiome ecosystem and improving the gut-immune axis. How to actually do this is a large topic in itself to save for another future blog post.
If you want to talk to me more about any part of this article, please contact me on info@nordicclinic.se or visit www.nordicclinic.se or www.nordicclinic.com to read more.
References
- Friedland, R. P., & Chapman, M. R. (2017). The role of microbial amyloid in neurodegeneration. PLoS pathogens, 13(12), e1006654. https://doi.org/10.1371/journal.ppat.1006654
- https://www.ncbi.nlm.nih.gov/pubmed/30508676
- https://science.sciencemag.org/content/366/6467/881.abstract
- https://www.sciencedirect.com/science/article/pii/S2211124720301674
- https://www.sciencedirect.com/science/article/pii/S0092867419308980
- https://genomemedicine.biomedcentral.com/articles/10.1186/s13073-016-0301-4
- Bates, D. W., Parsonnet, J., Ketchum, P. A., Miller, E. B., Novitsky, T. J., Sands, K., … & Kahn, K. (1998). Limulus amebocyte lysate assay for detection of endotoxin in patients with sepsis syndrome. Clinical infectious diseases, 27(3), 582-591.
- Yoseph, B. P., Klingensmith, N. J., Liang, Z., Breed, E. R., Burd, E. M., Mittal, R., Dominguez, J. A., Petrie, B., Ford, M. L., & Coopersmith, C. M. (2016). Mechanisms of Intestinal Barrier Dysfunction in Sepsis. Shock (Augusta, Ga.), 46(1), 52–59. https://doi.org/10.1097/SHK.0000000000000565
- Bergheim, I., Weber, S., Vos, M., Krämer, S., Volynets, V., Kaserouni, S., … & Bischoff, S. C. (2008). Antibiotics protect against fructose-induced hepatic lipid accumulation in mice: role of endotoxin. Journal of hepatology, 48(6), 983-992.
- Thuy, S., Ladurner, R., Volynets, V., Wagner, S., Strahl, S., Königsrainer, A., … & Bergheim, I. (2008). Nonalcoholic fatty liver disease in humans is associated with increased plasma endotoxin and plasminogen activator inhibitor 1 concentrations and with fructose intake. The Journal of nutrition, 138(8), 1452-1455.
- https://www.cochrane.org/CD012941/ARI_probiotics-healthy-bacteria-preventing-acute-middle-ear-infection-children
- Stamm, W. E., & Norrby, S. R. (2001). Urinary tract infections: disease panorama and challenges. The Journal of infectious diseases, 183(Supplement_1), S1-S4.
- Magruder, M., Sholi, A. N., Gong, C., Zhang, L., Edusei, E., Huang, J., … & Dadhania, D. M. (2019). Gut uropathogen abundance is a risk factor for development of bacteriuria and urinary tract infection. Nature communications, 10(1), 1-9.

